Signs and Symptoms of Breast Cancer

Breast cancer is most often associated with having a breast lump. However, your symptoms may vary depending on your specific type of breast cancer. While it’s true that many patients have a lump, it is possible to have breast cancer with no lump. So it’s important to know the other signs and symptoms
In general, the body produces certain warning signs. The most common is the breast lump, which may be located anywhere along your chest wall to under your armpit. You may have nipple bleeding or discharge, as well as related pain. There may be redness and/or swelling in any area of the breast or in one breast and not the other, and your nipple could look flatter or caved in.
Having some of these symptoms or breast changes doesn’t necessarily mean you have breast cancer. Many other factors go into a diagnosis, not just outward signs.
Early detection of breast cancer is key when it comes to breast cancer treatment options. If you have concerns with any new changes in your breasts, ask your doctor to review your symptoms and determine whether there’s a need for further evaluation.
Signs and Symptoms of Breast Cancer
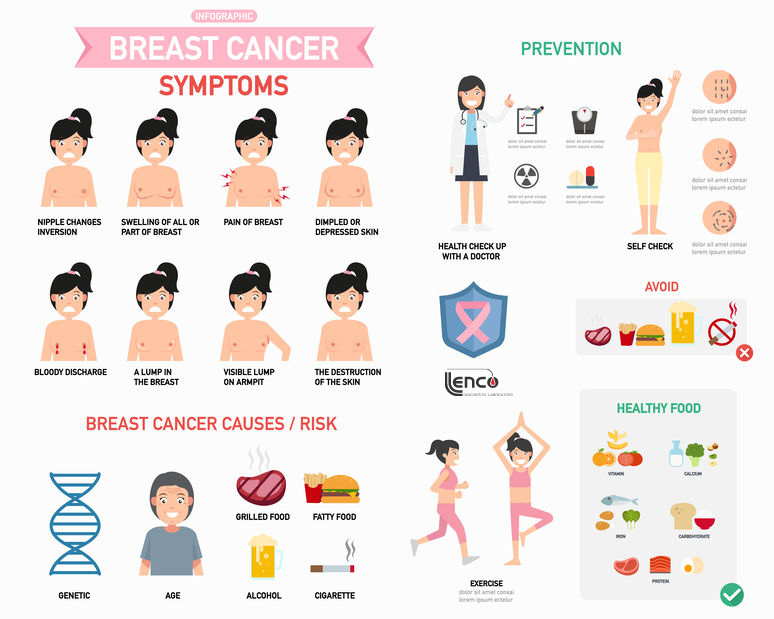
Symptoms
- A breast lump or thickening that feels different from the surrounding tissue
- Change in the size, shape or appearance of a breast
- Changes to the skin over the breast, such as dimpling
- A newly inverted nipple
- Peeling, scaling, crusting or flaking of the pigmented area of skin surrounding the nipple (areola) or breast skin
- Redness or pitting of the skin over your breast, like the skin of an orange
Inflammatory breast cancer symptoms
Unlike other breast cancers, inflammatory breast cancer (IBC) rarely causes breast lumps and may not appear on a mammogram. Inflammatory breast cancer symptoms include:
- Red, swollen, itchy breast that is tender to the touch
- The surface of the breast may take on a ridged or pitted appearance, similar to an orange peel (often called peau d’orange)
- Heaviness, burning, or aching in one breast
- One breast is visibly larger than the other
- Inverted nipple (facing inward)
- No mass is felt with a breast self-exam
- Swollen lymph nodes under the arm and/or above the collarbone
- Symptoms unresolved after a course of antibiotics
Causes
Doctors know that breast cancer occurs when some breast cells begin to grow abnormally. These cells divide more rapidly than healthy cells do and continue to accumulate, forming a lump or mass. Cells may spread (metastasize) through your breast to your lymph nodes or to other parts of your body.
Breast cancer most often begins with cells in the milk-producing ducts (invasive ductal carcinoma). Breast cancer may also begin in the glandular tissue called lobules (invasive lobular carcinoma) or in other cells or tissue within the breast.
Researchers have identified hormonal, lifestyle and environmental factors that may increase your risk of breast cancer. But it’s not clear why some people who have no risk factors develop cancer, yet other people with risk factors never do. It’s likely that breast cancer is caused by a complex interaction of your genetic makeup and your environment.
Risk factors
A breast cancer risk factor is anything that makes it more likely you’ll get breast cancer. But having one or even several breast cancer risk factors doesn’t necessarily mean you’ll develop breast cancer. Many women who develop breast cancer have no known risk factors other than simply being women.
Factors that are associated with an increased risk of breast cancer include:
- Being female. Women are much more likely than men are to develop breast cancer.
- Increasing age. Your risk of breast cancer increases as you age.
- A personal history of breast conditions. If you’ve had a breast biopsy that found lobular carcinoma in situ (LCIS) or atypical hyperplasia of the breast, you have an increased risk of breast cancer.
- A personal history of breast cancer. If you’ve had breast cancer in one breast, you have an increased risk of developing cancer in the other breast.
- A family history of breast cancer. If your mother, sister or daughter was diagnosed with breast cancer, particularly at a young age, your risk of breast cancer is increased. Still, the majority of people diagnosed with breast cancer have no family history of the disease.
- Inherited genes that increase cancer risk. Certain gene mutations that increase the risk of breast cancer can be passed from parents to children. The most well-known gene mutations are referred to as BRCA1 and BRCA2. These genes can greatly increase your risk of breast cancer and other cancers, but they don’t make cancer inevitable.
- Radiation exposure. If you received radiation treatments to your chest as a child or young adult, your risk of breast cancer is increased.
- Being obese increases your risk of breast cancer.
- Beginning your period at a younger age. Beginning your period before age 12 increases your risk of breast cancer.
- Beginning menopause at an older age. If you began menopause at an older age, you’re more likely to develop breast cancer.
- Having your first child at an older age. Women who give birth to their first child after age 30 may have an increased risk of breast cancer.
- Having never been pregnant. Women who have never been pregnant have a greater risk of breast cancer than do women who have had one or more pregnancies.
- Postmenopausal hormone therapy. Women who take hormone therapy medications that combine estrogen and progesterone to treat the signs and symptoms of menopause have an increased risk of breast cancer. The risk of breast cancer decreases when women stop taking these medications.
- Drinking alcohol. Drinking alcohol increases the risk of breast cancer.
