New treatment approach effectively treats the aggressive forms of prostate cancer
Researchers at the University of Chicago Medicine Comprehensive Cancer Center established “proof-of-concept” for a new treatment approach that was able to effectively treat the most aggressive forms of prostate cancer. The treatment showed complete tumor control and long-lasting survival without side effects in a mouse model of advanced prostate cancer.
Strategies to overcome resistance
“Prostate cancer in the metastatic setting is a hormonally driven disease, and thus is typically treated with androgen deprivation therapy (ADT) to lower testosterone levels,” said Akash Patnaik, MD, PhD, MMSc, an accomplished physician-scientist and internationally-recognized expert in prostate cancer research and treatment, who is the senior author of the publication. “Although this form of treatment has been shown to have significant anti-cancer responses in patients, the majority will become resistant to hormonal therapy, or castrate-resistant.”
Advanced prostate cancers that don’t respond to standard hormone-based therapy, chemotherapy and immunotherapy leave patients with very few options. The development of treatments for these aggressive cancers known as metastatic castrate-resistant prostate cancer (mCRPC) represents an area of critical unmet need.
Patnaik’s lab develops targeted therapeutic strategies to improve the responsiveness of prostate cancer to immunotherapy. They discovered that the immune system can often promote the growth of cancer -; instead of suppressing it -; through recruitment of abnormal tumor-associated macrophages that express PD-1 (a checkpoint molecule which turns off an anti-cancer immune response) into the tumor microenvironment.
In a study published in March 2023, Patnaik and colleagues found that co-targeting the PI3K and PD-1 pathway enhanced the antitumor effects of ADT in PTEN-deficient prostate cancer, which is an aggressive form of advanced prostate cancer that results from the loss of a particular gene that keeps cell growth in check.
However, they observed that their strategy significantly enhanced the response rate for 60% of the mice, but 40% remained resistant to the therapy. The team conducted follow-up studies and found that activation of Wnt/β-catenin pathway restored lactate production in the treatment-resistant cancers, which they discovered drives the tumor-promoting properties of macrophages.
T cell activation
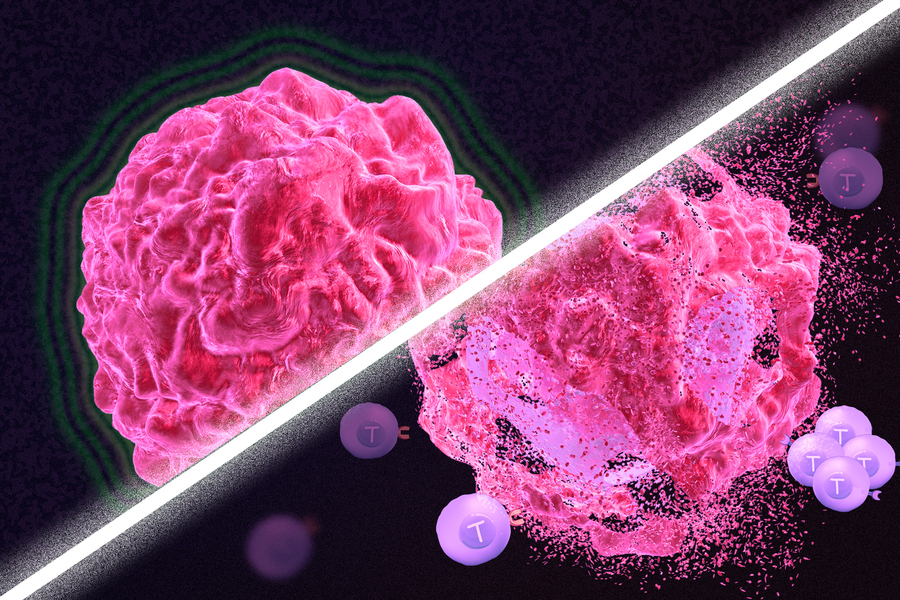
One class of drugs currently used for cancer immunotherapy is checkpoint blockade inhibitors, which take the brakes off of T cells that have become “exhausted” and unable to attack tumors. These drugs have shown success in treating a few types of cancer but do not work against many others.
The drugs that appear to work best with this approach are drugs that cause DNA damage. The researchers found that when DNA damage occurs in tumor cells, it activates cellular pathways that respond to stress. These pathways send out distress signals that provoke T cells to leap into action and destroy not only those injured cells but any tumor cells nearby.
